Understanding Genetic Testing for Prostate Cancer Detection
This article explores the role of genetic testing in prostate cancer detection, highlighting recent advances, risk factors, and the clinical utility of gene screening. It provides insights into how genetics can help in early diagnosis and personalized treatment, emphasizing the importance of family history and targeted genetic tests.
Sponsored

Recent advancements in genetic medicine have significantly improved our ability to detect and prevent prostate cancer. Discussions continue about the pros and cons of genetic testing and its role in early identification of the disease.
The discovery of the DNA double helix in 1953 revolutionized human genetics, offering deep insights into disease mechanisms. The human genome provides vital information that can aid in understanding, preventing, and treating prostate cancer through genetic testing.
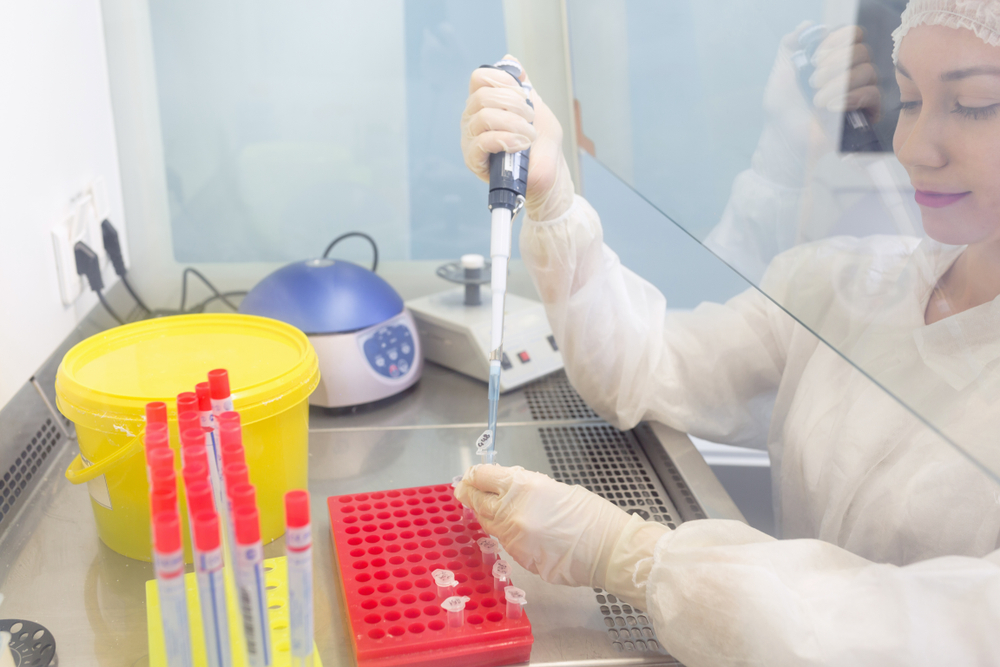
Genetic screening for prostate cancer
Genetic testing offers numerous advantages, including personalized treatment strategies for diagnosed individuals and early detection for those at risk.
However, questions remain about the effectiveness of prostate cancer DNA testing for screening and prevention. Experts note that such tests are mainly recommended for men with specific risk factors but are not universally applicable to men with a family history of breast or ovarian cancers.
Prostate cancer risk factors and genetic insights
Key elements of genetic testing involve detailed family history, assessment of risk factors, and considerations for individuals with multiple affected relatives. It’s estimated that about 1 in 9 American men will develop prostate cancer during their lifetime.
Family history assessment considers cancer in paternal and maternal lines, primary diagnoses, ethnicity, race, and other health conditions like benign prostatic hypertrophy. Currently, multigene tests targeting prostate cancer susceptibility are increasingly utilized in healthcare settings, aiding both in diagnosis and genetic counseling.