Understanding the Reasons Behind Hemoptysis
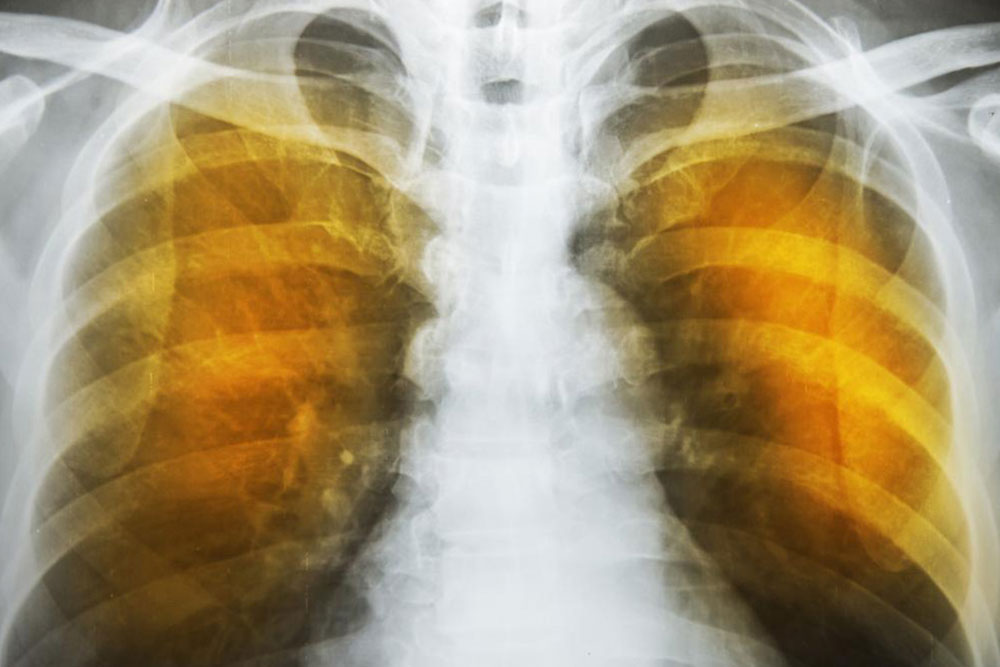
Hemoptysis, or coughing up blood, can indicate minor or serious health issues. Causes range from infections to critical conditions like lung cancer or tuberculosis. Recognizing symptoms and seeking prompt medical help are crucial for effective treatment and prevention of complications.
Sponsored

Seeing blood when you cough can be shocking, regardless of the amount. Hemoptysis, or coughing up blood, may signal a significant health issue. The bleeding source could be your throat, upper airways, lungs, or nose.
The presence of blood during coughing indicates an underlying condition. Its severity depends on the volume of blood and how long the episodes last. Blood mixed with mucus and air appears frothy or bubbly, typically bright red but sometimes rust-colored.
Causes of Hemoptysis
Hemoptysis can result from various factors, ranging from infections to malignant conditions.
Common causes include:
Minor respiratory infections
Chronic obstructive pulmonary disease (COPD)
Asthma
Throat infections
More serious conditions associated with significant bleeding are:
Chest trauma or injury
Inhalation of foreign objects
Lung tumors
Tuberculosis
Cystic fibrosis
Pulmonary embolism
Damage to lung arteries
Medical procedures such as spirometry, laryngoscopy, nasal surgery, or airway biopsies can also cause minor bleeding episodes.
These often resolve quickly and aren't usually a concern.
What does coughing up blood indicate?
The health implications depend on the cause. Seek emergency care if you experience:
Bleeding after chest injury
Large amounts of blood (over a few teaspoons)
Blood in urine or stool
Dizziness, light-headedness, or difficulty breathing post-bleeding
Immediate medical attention is vital for hemoptysis. Consulting a doctor, undergoing examinations, and diagnostics are essential for identifying the cause. Severe bleeding can be life-threatening if untreated.