Understanding Asthma: Causes, Mechanisms, and Immune Factors
This article explores the underlying causes, mechanisms, and immune responses involved in asthma, highlighting the differences between acute attacks and chronic inflammation. It covers common triggers, the immune pathways involved, and strategies to manage and prevent symptoms effectively.
Sponsored
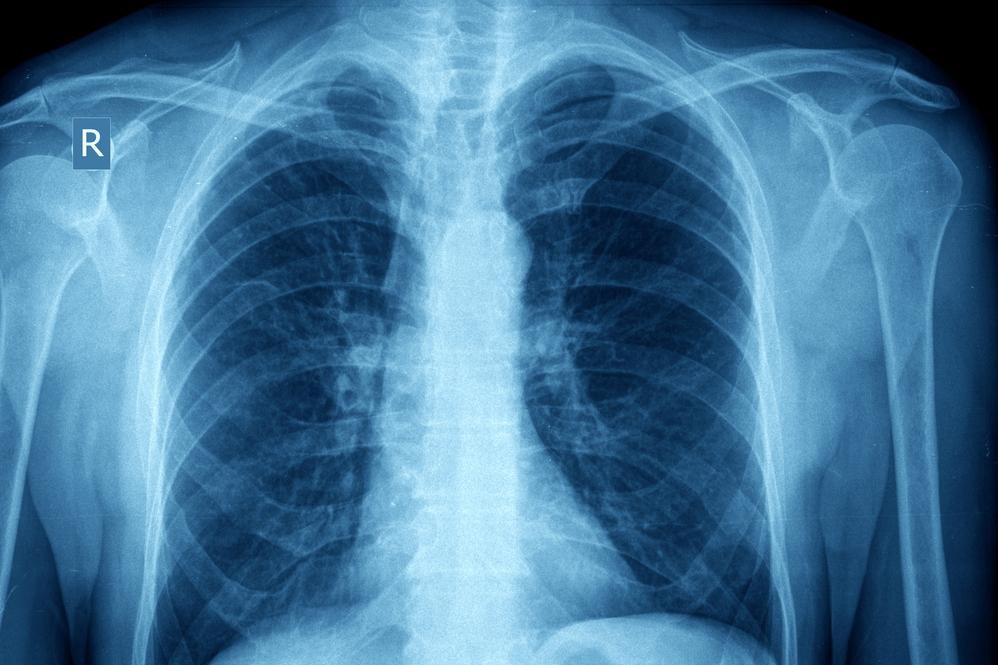
Asthma manifests in two primary forms: sudden episodes and long-term condition. Sudden episodes, called asthma attacks, occur when triggers provoke airway constriction, leading to rapid symptoms. The chronic form results from persistent inflammation, causing structural lung changes over time.
Asthma Attack
Exposure to triggers causes airway muscles to tighten, reducing airflow, while airway linings swell and produce excess mucus. Symptoms include difficulty breathing, coughing, chest tightness, and wheezing.
Chronic asthma involves ongoing airway inflammation, increasing sensitivity to various triggers. Managing the condition effectively can reduce lung damage. Common triggers encompass physical activity, infections, environmental pollutants, irritants like smoke or perfumes, emotional stress, allergens (such as pollen, dust, pet dander), cold air, gastric reflux, and certain medications like NSAIDs.
Triggers may cause airway inflammation, constriction, or both. The immune response in asthma involves complex interactions, notably Th1, Th2, and IgE pathways. Even healthy individuals can experience exercise-induced bronchoconstriction (EIB), which can be mitigated with pre- and post-exercise medications.
Immune System's Role in Asthma
Asthma’s development is closely tied to immune responses. Th2 immune responses, which are dominant in allergies, lead to increased IgE production. IgE binds to allergens and mast cells, leading to histamine release, inflammation, and mucus overproduction, contributing to airway narrowing and symptom development.






