Comprehensive Guide to Varicose Vein Specialists: Treatments and Patient Care
This comprehensive guide explores the role of varicose vein specialists, detailing their diagnosis methods, treatment options like sclerotherapy and laser therapy, and the importance of choosing experienced practitioners for optimal care. It emphasizes minimally invasive treatments and patient follow-up to ensure effective management of varicose veins, ultimately improving life quality and health outcomes.
Sponsored

Varicose veins are enlarged, twisted veins that often appear on the legs, leading to discomfort, soreness, and other health issues. Although many see them as merely cosmetic, these veins can interfere with daily life and cause complications like ulcers or blood clots. Seeking the expertise of specialized vein doctors is essential for effective management.
Who are Varicose Vein Experts?
These specialists are trained healthcare professionals skilled in diagnosing and treating venous disorders, typically coming from backgrounds in vascular surgery, radiology, or phlebology—the medical field focusing on veins.
Their main goal is to ease symptoms, enhance cosmetic appearance, and prevent serious complications related to varicose veins.
Role of Varicose Vein Specialists
Diagnosis
Accurate diagnosis involves evaluating medical history, conducting physical exams, and utilizing imaging tests like Doppler ultrasounds to determine the extent of vein issues. These images reveal problems such as venous reflux, caused by malfunctioning valves that allow blood to flow backwards.
Treatment Options
Depending on the severity, specialists offer various personalized treatments:
Sclerotherapy
Sclerotherapy is a minimally invasive injection procedure that causes small to medium veins to collapse and fade, ideal for spider veins and smaller varicose veins.
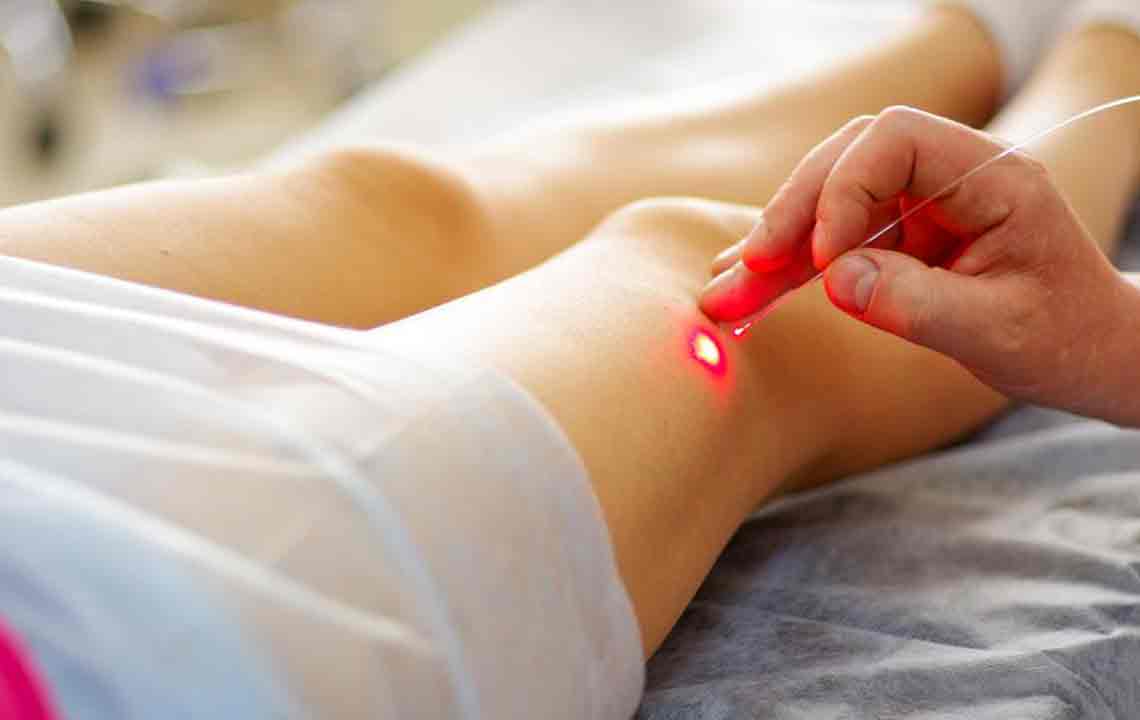
Endovenous Laser Therapy (EVLT)
EVLT uses laser energy to seal problematic veins by inserting a tiny laser fiber through the skin, redirecting blood flow to healthier veins.
Radiofrequency Ablation (RFA)
RFA employs radio waves to heat and close varicose veins, offering quick recovery and high success rates.
Ambulatory Phlebectomy
This surgical technique removes large, bulging veins via small skin incisions, usually under local anesthesia.
Compression Therapy
Wearing compression stockings supports blood flow, often combined with other treatments for symptom relief.
Follow-Up and Patient Guidance
Post-treatment care includes lifestyle modifications such as regular exercise, weight control, and avoiding long periods of standing or sitting. Follow-up visits enable specialists to monitor progress and manage any ongoing issues.
How to Choose a Varicose Vein Specialist
Optimal results depend on selecting experienced practitioners. Consider these factors:
Qualifications and Experience
Look for board-certified specialists with a focus on vein conditions and proven experience in varicose vein treatments.
Patient Feedback
Reading reviews can offer insights into their expertise, patient satisfaction, and quality of care.
Available Treatments
Ensure they provide a variety of treatment options tailored to individual needs.
Communication and Consultation
A good doctor will thoroughly explain the condition, treatment plans, and answer questions clearly.
Varicose veins are more than just a cosmetic issue; they can impact overall health and quality of life. Skilled vein specialists diagnose, treat, and support patients through minimally invasive procedures designed to relieve symptoms, improve appearance, and prevent complications. Selecting a qualified, experienced professional ensures effective management and a healthier, more comfortable life.