Understanding Neutrophils and Their Role in Immune Defense
This article explores the vital role of neutrophils in human immunity, detailing their production, functions, and how they defend against bacterial infections. It also covers conditions like neutropenia, highlighting causes and implications for health and disease management.
Sponsored
Neutrophils in the Human Immune System
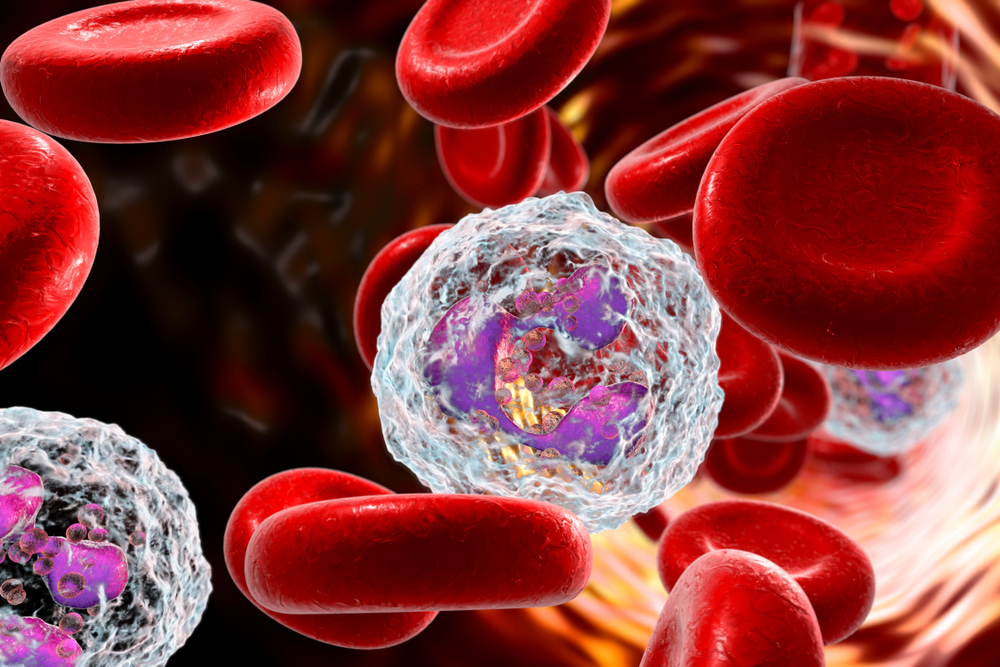
Most people are familiar with neutrophils, especially when reviewing blood test results that include differential counts. Blood comprises mainly red blood cells, or erythrocytes, which give the blood its red hue, and white blood cells, or leucocytes, which are vital for defending against pathogens like bacteria and viruses. Among white blood cells, neutrophils are the most abundant, making up 40% to 70% of leukocytes.
If levels fall below this range, it is termed neutropenia. Neutrophils act as initial responders during bacterial invasions and toxins.
Where Are Neutrophils Formed?
Produced in the bone marrow within long bones and the pelvis.
Approximately 55-60% of bone marrow activity is dedicated to neutrophil production.
They circulate in the blood for 5 to 90 hours before moving into tissues, lasting around 2 days within cells.
Daily production is about 10^11 neutrophils, increasing to 10^12 during infections.
Why Do We Call Them Neutrophils?
Their name stems from the neutral pink stain they take up during microscopic examination, using standard dyes.
Their production rate highlights their critical role in fighting bacterial pathogens, increasing significantly during infections.
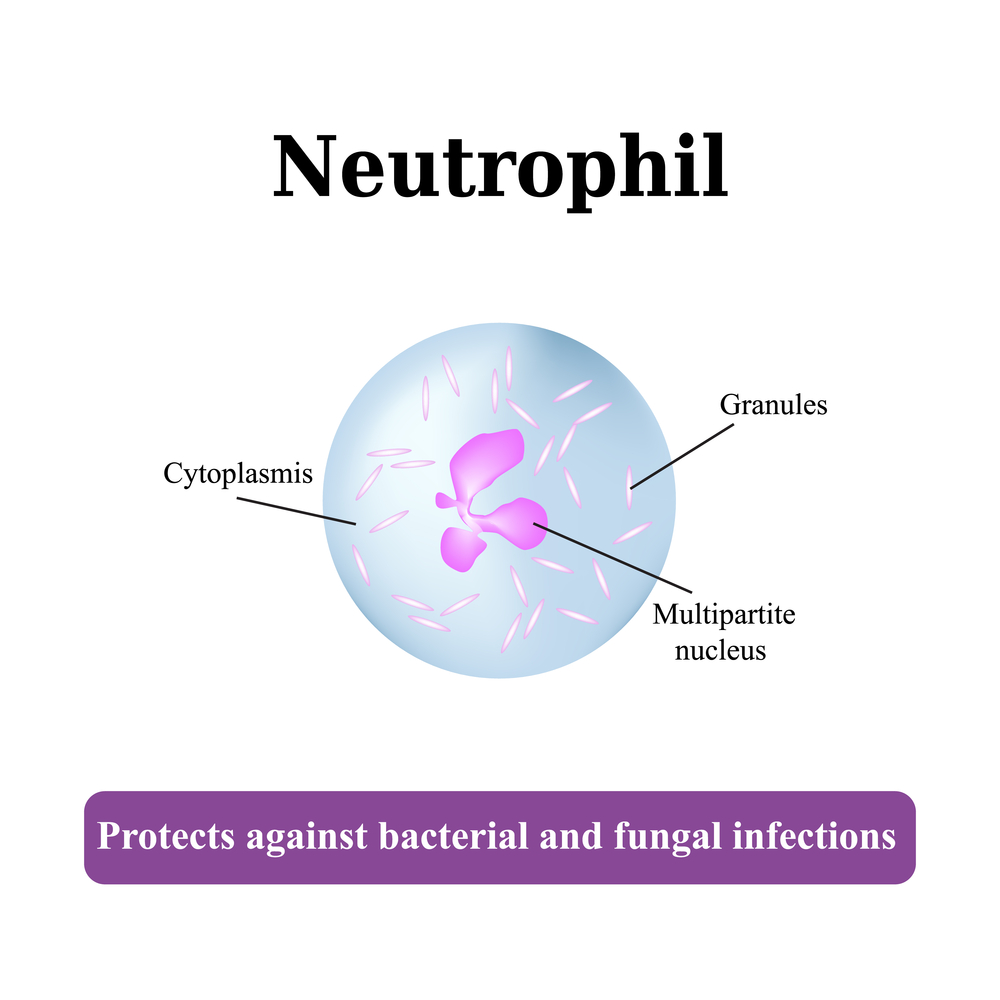
They feature a nucleus with 2 to 5 lobes, and abnormal hyper-segmentation may indicate certain health issues like vitamin B12 deficiency.
Characteristics of Neutrophils
Size typically ranges from 12 to 15 microns, shrinking to about 9 microns in blood circulation.
Part of the granulocyte group, sharing a lobed nucleus with eosinophils and basophils.
Their lobed nuclei are connected by chromatin strands, with nuclear disappearance as they mature, a rare process among cells.
How Do Neutrophils Combat Bacterial Invaders?
They rapidly migrate to infection sites, passing through blood vessel walls into tissues.
Migration involves extending pseudopodia with chemical receptors, following signals to reach infection zones.
This process, called neutrophil swarming, involves coordinated movement of large cell groups.
Once at the site, they engulf bacteria through phagocytosis, releasing destructive chemicals via degranulation.
Neutrophils produce extracellular traps (NETs)—net-like chromatin structures with antimicrobial factors—that trap and kill bacteria.
They also activate other immune cells, initiating a comprehensive immune response.
However, in autoimmune diseases, neutrophil activity may sometimes worsen inflammation.
What Is Neutropenia?
Conditions where neutrophil counts fall below normal are called neutropenia.
Common causes include chemotherapy, radiation therapy, certain infections like hepatitis, HIV/AIDS, malaria, sepsis, and autoimmune disorders.
Medications and hypersplenism can also contribute to low neutrophil levels, increasing infection risk.