Identifying the Signs and Symptoms of Diverticulitis
This article details how to identify diverticulitis through symptoms like lower abdominal pain, changes in bowel habits, and bleeding. It explains the causes, including low-fiber diets, and emphasizes the importance of diagnosis via physical exams and imaging tests. Treatment varies based on severity, with home care for mild cases and medical interventions for advanced symptoms. Recognizing early signs and seeking prompt medical attention can prevent serious complications.
Sponsored
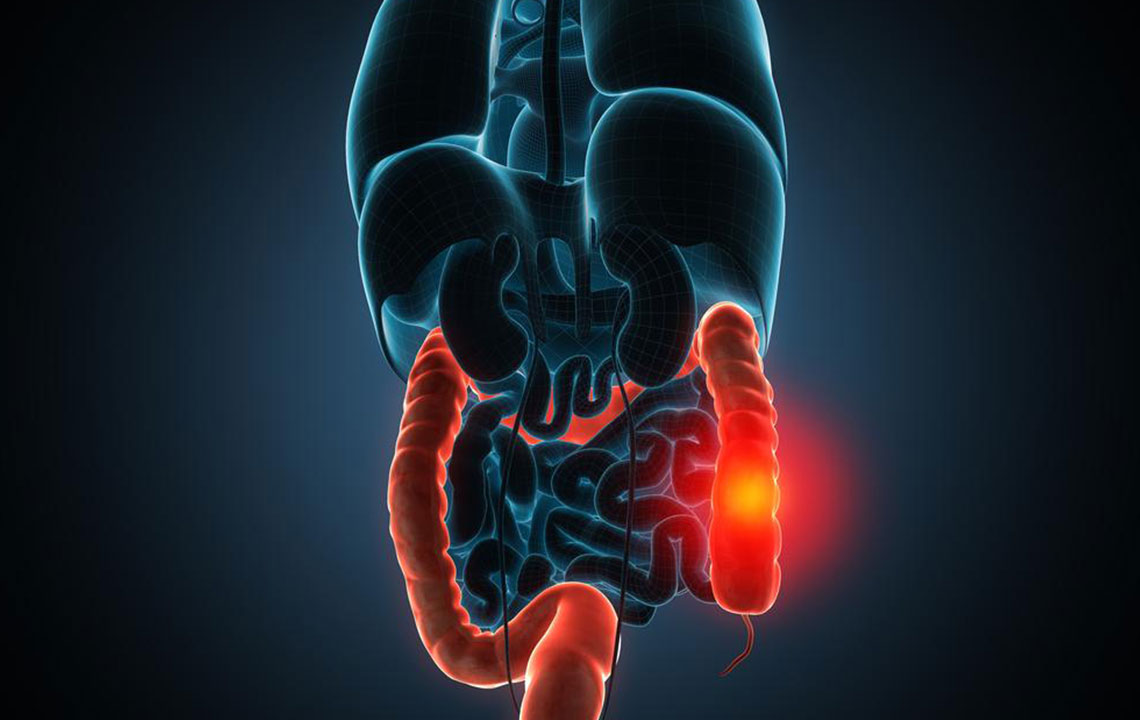
Recognizing the Indicators of Diverticulitis
Diverticulitis refers to inflammation or infection of small pouches called diverticula that develop in the lining of the large intestine or colon. Initially, these pouches are known as diverticulosis, but when they become inflamed or infected, the condition is labeled as diverticulitis.
Underlying Causes
Most often affecting older adults, the exact cause of diverticulosis remains uncertain. However, a diet low in fiber is believed to promote the formation of diverticula. Without sufficient fiber to add bulk, the colon must exert more pressure to move stool, leading to diverticula formation. Consuming a fiber-rich diet and staying well-hydrated can help soften stool and reduce the risk of developing diverticulitis.
Common symptoms include persistent pain in the lower left abdomen, starting below the navel and moving to the left side. The pain often intensifies after meals and may be relieved by bowel movements. Other long-term signs are altered bowel habits, bloating, loss of appetite, nausea, and fever exceeding 38°C (100.4°F). Bright red or dark rectal bleeding can occur but typically resolves on its own. If not treated, diverticulitis can lead to complications such as increased pain, persistent fever, vomiting, constipation, abdominal distension, and urinary discomfort. Severe cases demand immediate medical attention, especially if bleeding or intense abdominal pain arise. While weight loss isn't directly related, ongoing symptoms like rectal bleeding or frequent bowel issues necessitate a healthcare visit.
How Diverticulitis is Diagnosed
Diagnosis involves assessing symptoms and conducting physical exams. A doctor may perform digital rectal examinations to check for blood or pain, alongside blood tests to detect elevated white blood cell counts indicative of infection. Imaging scans like CT scans help visualize inflamed diverticula. Endoscopic procedures such as colonoscopy or sigmoidoscopy offer direct views of the colon's interior, aiding definitive diagnosis. These tests are generally well-tolerated and crucial in confirming diverticulitis.
Managing Diverticulitis
The treatment plan depends on symptom severity. Mild cases often require home care, including bed rest, a liquid diet to allow the intestine to heal, and careful use of prescribed antibiotics and pain relievers. Gradual reintroduction of solid foods follows medical advice. Recovery can span weeks to months, with lifestyle and dietary modifications supporting healing and preventing future episodes.