Understanding Elevated Monocyte Levels: Causes, Signs, and Care
Elevated monocyte counts, or monocytosis, can signal infections, autoimmune issues, or blood disorders. This article explains causes, symptoms, diagnosis options like blood tests, and treatment strategies. Maintaining a healthy lifestyle through diet, exercise, and stress management can support immune health. Medical consultation is essential for proper diagnosis and care. Understanding these aspects helps in timely intervention and improved health outcomes.
Sponsored

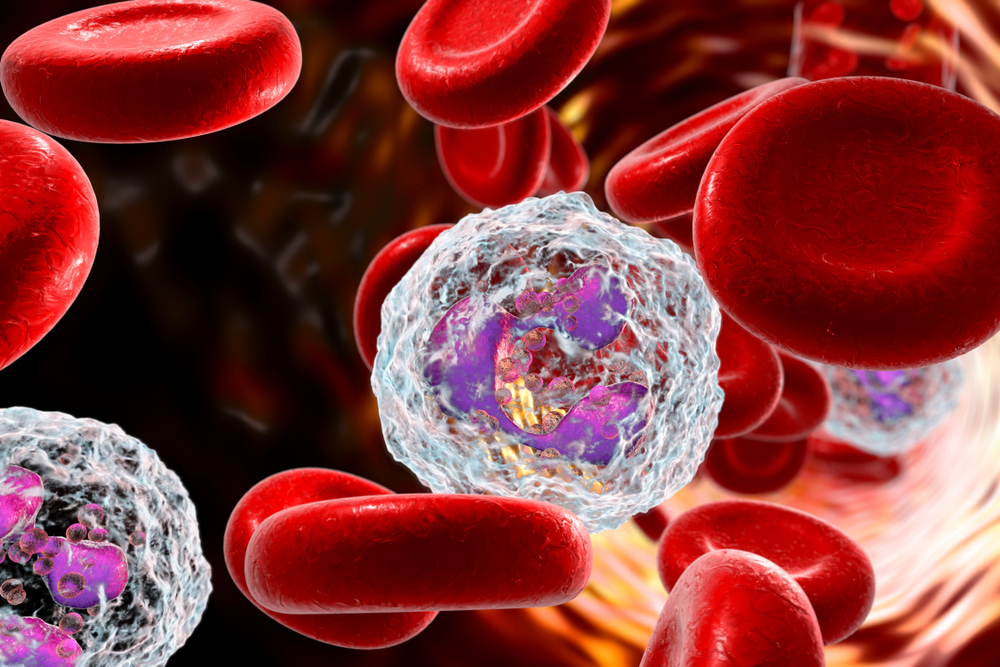
Monocytes are a subtype of white blood cells that play a vital role in fighting infections, removing dead cells, and supporting immune defense. Normally, they account for about 2-8% of total white blood cells, roughly 100 to 700 cells per mm3. When their numbers increase beyond normal, the condition is known as monocytosis. This may signal underlying infections, autoimmune issues, blood disorders, or certain cancers.
What is monocytosis?
It is characterized by an abnormally high monocyte count, often related to infections, immune responses, or hematological conditions.
Various conditions such as endocarditis, tuberculosis, malaria, autoimmune disorders, sarcoidosis, certain infections, blood marrow recovery, chronic stress, heart attacks, splenectomy, and blood cancers can cause increased monocyte levels.
Symptoms of elevated monocytes
Many individuals with high monocyte counts do not display noticeable symptoms. When present, symptoms often relate to the underlying cause and may include:
Fatigue
Weakness
Swelling
Fever
To identify an elevated monocyte level, healthcare providers order blood tests that examine different white blood cell types. Normal values for other white cells are as follows:
Basophils produce histamine and constitute 0.5-1% of white blood cells.
Eosinophils help combat parasites and support allergic reactions, making up 1-4%.
Lymphocytes, responsible for antibodies, form 20-40%,
Neutrophils, the body's primary bacteria fighters, account for 55-70%,
Immature band neutrophils are 0-3%, aiding infection response and healing.
A monocyte level exceeding 10% (or 800/mm3) suggests an immune response to underlying issues.
Diagnosis and Management
Doctors may recommend further tests based on symptoms, including X-rays, blood and urine analysis, cultures, or bone marrow examination. These help pinpoint the cause of monocytosis. Common tests include:
Complete Blood Count (CBC)
Analyzes overall white blood cell levels in the blood.
Blood Smear
Microscopic examination of blood cells to evaluate their shape and size.
Absolute Monocyte Count
Calculates monocyte numbers by multiplying their percentage in CBC with total white blood cells.
Treatment hinges on addressing the underlying cause. Options may include antiviral or antibiotic therapies, cancer treatments like chemotherapy or stem cell transplants, or medications targeting parasitic infections. In some cases, regular blood monitoring is necessary for conditions like leukemia.
Ways to Support Healthy Monocyte Levels
Beyond medical intervention, lifestyle changes can promote immune health:
Exercise Regularly
Consistent physical activity can help maintain balanced monocyte counts and improve overall health.
Consume Anti-inflammatory Foods
Foods like leafy greens, berries, nuts, fatty fish, and olive oil can reduce inflammation and support immune regulation. Avoid processed foods, high-sugar drinks, and fried items.
Manage Stress and Rest Adequately
Reducing stress and getting sufficient sleep can help stabilize immune function and monocyte levels.
If monocyte levels are elevated, consulting a healthcare provider is recommended to determine the underlying condition and appropriate treatment plan.