Managing Vaginal Atrophy: Symptoms, Causes, and Treatment Options
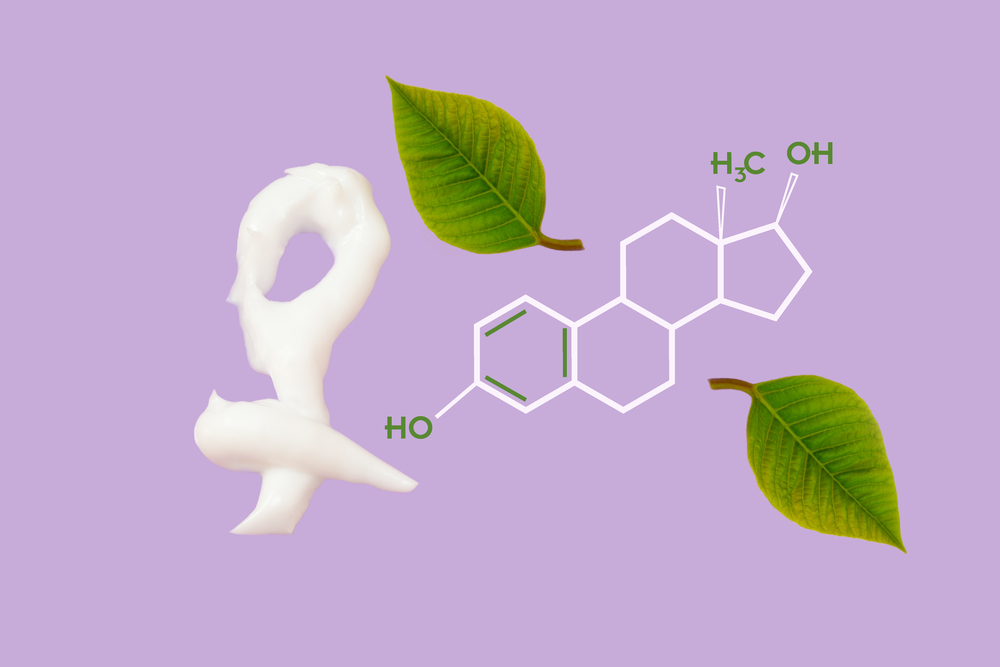
This article explores vaginal atrophy, highlighting its symptoms, causes, diagnosis, and treatment options. It emphasizes the importance of understanding this condition that affects many women post-menopause. Available management strategies include moisturizers, lubricants, and localized estrogen therapies, providing relief from dryness, discomfort, and urinary issues. Early diagnosis and appropriate treatment can significantly improve quality of life for women experiencing this common age-related condition.
Sponsored

Understanding Vaginal Atrophy and Its Treatment
Vaginal atrophy is a common condition linked to aging that primarily affects women around menopause, though it can occur earlier. It results from fluctuating estrogen levels, which influence the health of vaginal tissues, skin, and muscles. Even after menopause, estrogen persists in the body but in reduced amounts. The decline causes thinning and loss of elasticity in vaginal walls, leading to discomfort and dryness.
This condition narrows the vaginal canal, causes dryness, and can be associated with urinary issues such as burning or infections. When including urinary symptoms, it is classified as Genitourinary Syndrome of Menopause (GSM).
What is Vaginal Atrophy?
Primarily associated with aging, though hormonal changes can occur anytime.
The close relationship between the urinary and genital systems means that vaginal atrophy can affect urinary health.
The condition's manifestations include increased risk of urinary infections and thinning of vaginal tissues.
Common Signs and Symptoms
Signs include dryness, itching, burning, discomfort during intercourse, and occasional bleeding after sex.
Urinary signs involve burning during urination, incontinence, painful urination, and frequent infections.
Prevalence and Risk Factors
Between 40-50% of postmenopausal women experience GSM, though only a fraction seek medical help.
Factors like smoking, which impairs blood flow and reduces estrogen efficacy, increase risk.
Women with regular childbirth and active lifestyles are less prone, as sexual activity promotes healthy blood circulation.
Diagnosis Methods
Medical history review and pelvic exams are essential for diagnosis.
Tests such as urine analysis and vaginal pH testing help assess the condition further.
Available Treatments
While a complete cure is unavailable, symptoms can be managed effectively.
Hormone Replacement Therapy (HRT) use has decreased due to associated risks.
Vaginal moisturizers provide hydration and can be applied every few days.
Over-the-counter water-based lubricants are preferred; mineral oil or glycerin-based products may cause irritation.
Localized estrogen therapies, including creams and vaginal rings, offer targeted relief with fewer systemic risks.
Topical estrogen creams require daily application initially, then reduced frequency; vaginal rings deliver hormones over months.