Understanding Vaginal Atrophy: Causes, Symptoms, and Management Options
This article provides a comprehensive overview of vaginal atrophy, its symptoms, risk factors, diagnosis, and available treatment options. It discusses hormonal influences, emerging therapies like SERMs, and lifestyle considerations to help women manage this common condition effectively. Understand the causes and latest treatments to improve quality of life during menopause and beyond.
Sponsored
Insights into Vaginal Atrophy and Its Remedies
“Appreciate what you have while striving for more.” – Helen Keller
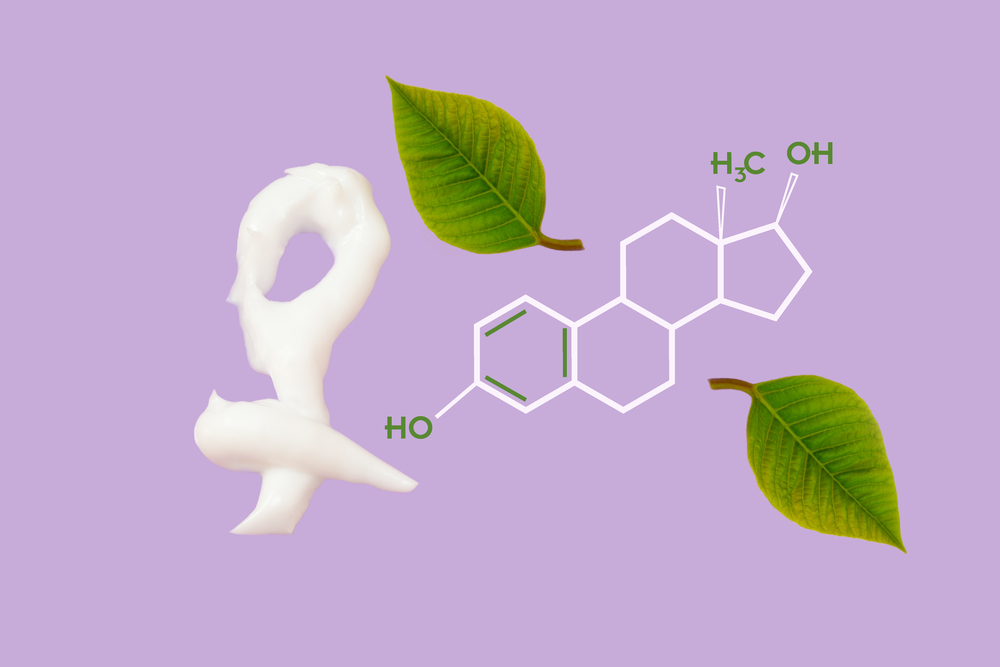
Vaginal atrophy, commonly observed after menopause, is linked to aging and changes in the reproductive system. Although often associated with menopause, it can occur at any age due to fluctuating estrogen levels, which are present from menarche onwards. This condition also impacts the urinary system, leading to the broader term “genitourinary syndrome of menopause (GSM).” Current treatments are limited, motivating ongoing research to find more effective, lasting solutions.
What is Vaginal Atrophy?
It involves thinning and loss of elasticity of the vaginal walls and muscles.
This results in reduced lubrication, increased pain during sex (dyspareunia), and discomfort.
Prevalence of GSM
Estimating its occurrence is challenging since many women do not seek medical help due to lack of awareness.
Most are unaware that symptoms relate to hormonal changes related to aging.
Symptoms Associated with Vaginal Atrophy
Common signs include dryness, burning, itching, abnormal discharge, painful intercourse, and light bleeding after sex.
Urinary issues such as painful urination, burning sensation, frequent urination, and incontinence often accompany the condition.
Psychological effects may involve feelings of unattractiveness, insecurities, and depression in severe cases.
Factors That Increase Risk
The primary factor is hormonal decline during menopause.
Smoking impairs blood flow and reduces the effectiveness of estrogen.
Medications like contraceptives and breastfeeding may contribute.
C-section deliveries, which diminish vaginal circulation, also raise risk.
Sexual inactivity, autoimmune diseases like Sjögren's syndrome, and diabetes can exacerbate symptoms.
Diagnostic Methods
Doctors perform pelvic examinations and review medical history to exclude other abnormalities.
Urinary symptoms are evaluated to differentiate from other conditions.
Vaginal pH levels are tested through vaginal fluid sampling or acidity tests.
Available Treatment Strategies
While a permanent cure remains elusive, various treatments can manage symptoms effectively.
Hormone therapy has fallen out of favor due to associated risks.
Topical moisturizers and lubricants provide relief; natural oils are also used but may cause allergies.
Estrogen creams, tablets, or vaginal rings are common, with higher doses risking systemic effects.
Regular sexual activity stimulates blood flow and can mitigate symptoms.
Emerging therapies include local androgen treatment, with recent research exploring testosterone’s role in vaginal health.
Research on Selective Estrogen Receptor Modulators (SERMs)
Recent studies focus on SERMs for their potential to treat menopausal symptoms and protect breast and uterine tissues.
These tissue-specific estrogen regulators are promising but require further investigation.






