Comprehensive Guide to Managing and Treating a Herniated Spinal Disc
Learn about herniated disc symptoms, causes, and treatments in this comprehensive guide. Discover conservative approaches like physical therapy and exercises, and understand when surgery may be necessary. Early intervention can prevent serious nerve damage and restore spinal health effectively.
Sponsored
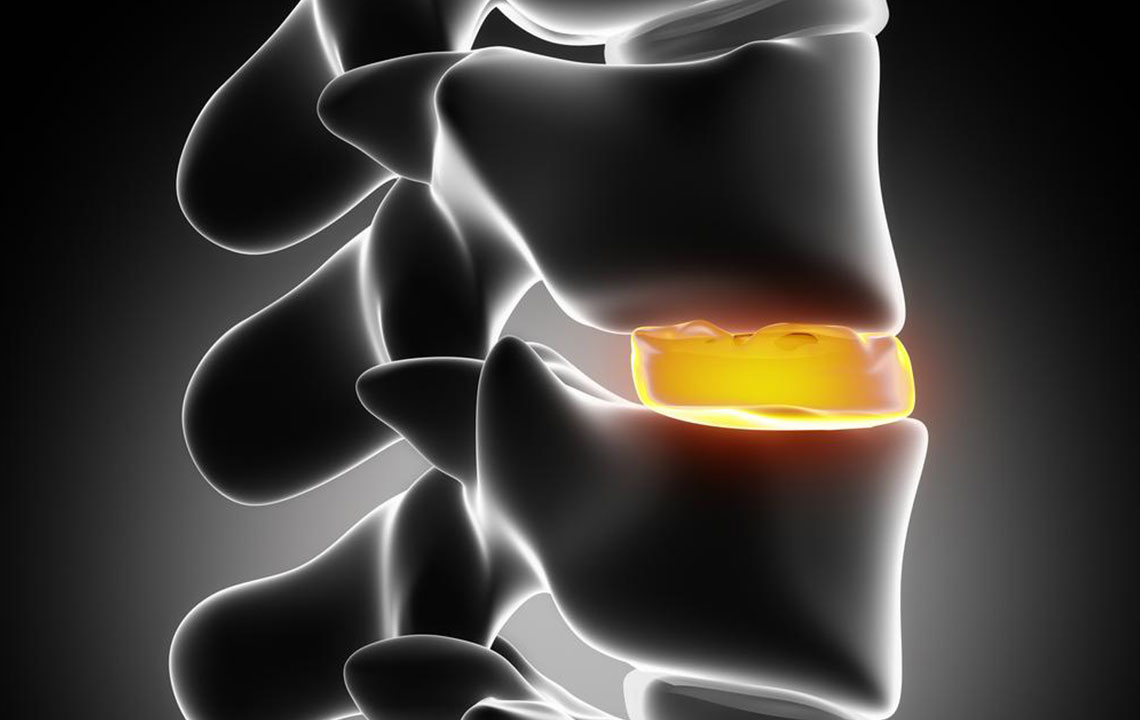
Understanding Herniated Disc: Symptoms, Causes, and Treatment Options
A herniated disc, also known as a slipped or ruptured disc, may cause symptoms like numbness, weakness, or tingling in the legs or arms. This condition occurs when the disc between vertebrae protrudes beyond its normal boundary, pressing on nearby nerves. Often painless, it can nevertheless lead to discomfort if untreated. Herniated discs are common in the cervical, thoracic, and lumbar regions of the spine. The discs act as shock absorbers, with an outer annulus fibrosus and inner nucleus pulposus. Damage to the disc’s outer layer allows internal material to press against nerves, leading to pain and neurological issues.
Spinal discs are vital structures composed of glycoprotein and fibrocartilage, providing cushioning and flexibility to the spine. When the annulus fibrosus sustains injury or degenerates, the risk of herniation increases. Traumatic events, repetitive microtrauma, or genetic factors can weaken these discs. A herniated disc may cause symptoms such as localized pain, numbness, muscle weakness, and nerve pressure effects like tingling or radiating discomfort. Symptoms vary depending on the affected spinal region, with cervical herniations causing neck and arm pain, while lumbar ones can lead to leg pain and weakness.
Common causes include accumulated minor injuries over time, sudden excessive pressure like falls or accidents, and hereditary predispositions. Symptoms often develop gradually and may worsen with certain activities. In some cases, nerve compression can cause bowel or bladder changes or paralysis.
Initial treatment often involves conservative methods without surgery. This includes pain relief, inflammation management, physical therapy, and exercises to restore mobility and strengthen supporting muscles. The process typically unfolds in four stages:
Phase 1: Pain Management and Protection - Using ice, medications, and therapies like acupuncture to reduce inflammation and ease discomfort.
Phase 2: Functional Restoration - Focused on improving joint alignment, muscle strength, and flexibility through targeted exercises, core strengthening, and massage.
Phase 3: Full Function Recovery - Enhancing control over back movements, strengthening pelvis, spine, and leg muscles, progressing from walking to more intense activities based on individual capacity.
Phase 4: Prevention of Recurrence - Maintaining back health through personalized routines designed to avoid future injuries and manage lifestyle factors.
Despite conservative approaches, some cases require surgical intervention. Surgical options depend on the herniation’s location and severity. Early diagnosis and treatment are essential to prevent long-term nerve damage and functional impairment. A herniated disc can be effectively managed with proper care, so prompt medical attention is recommended.






